Children
Unexplained bruises in children, particularly infants who are not mobile, are a red flag and merit immediate evaluation for potential abuse or underlying medical disorders. Bruising over the ears, neck, trunk, or patterns like hand‑prints or belt‑marks should prompt urgent investigation. Pediatric conditions like ITP, leukemia, or vascular malformations should be ruled out.
Elderly
Thinning skin and fragile capillaries, often worsened by sun damage and corticosteroids, cause easy bruising. Aging skin also heals more slowly. Fall risk and poor vision compounds bruising risks. However, unexplained or large bruises still warrant evaluation, especially to rule out bleeding disorders or medication side effects.
Pregnancy
Pregnancy induces many changes: increased blood volume, altered platelet function, and potential for gestational thrombocytopenia. Additionally, increased falls or accidents due to changes in balance may cause bruises. However, unexplained bruising should prompt evaluation for preeclampsia‑related coagulopathy or undiagnosed bleeding disorders.
Signs That Warrant Immediate Medical Attention
If bruising is accompanied by any of the following, seek emergency care: significant bleeding that doesn’t stop after 10–15 minutes deep muscle or joint pain and swelling infected-appearing or rapidly spreading bruise signs of anemia (pallor, rapid heart rate, fainting) …or systemic symptoms such as fever, fatigue, night sweats, weight loss If there is a history of abuse or you suspect foul play, it is ethically and legally important to involve appropriate protective services.
How Doctors Evaluate Unexplained Bruises
History
A detailed history includes onset, frequency, size, and location of bruises; any associated symptoms (bleeding gums, nosebleeds, joint pain); medication use (including supplements/herbals); personal or family history of bleeding disorders; alcohol use and liver disease; nutritional status and dietary habits; history of injuries or falls; in children, careful social context evaluation; in elderly, fall risk and home environment.
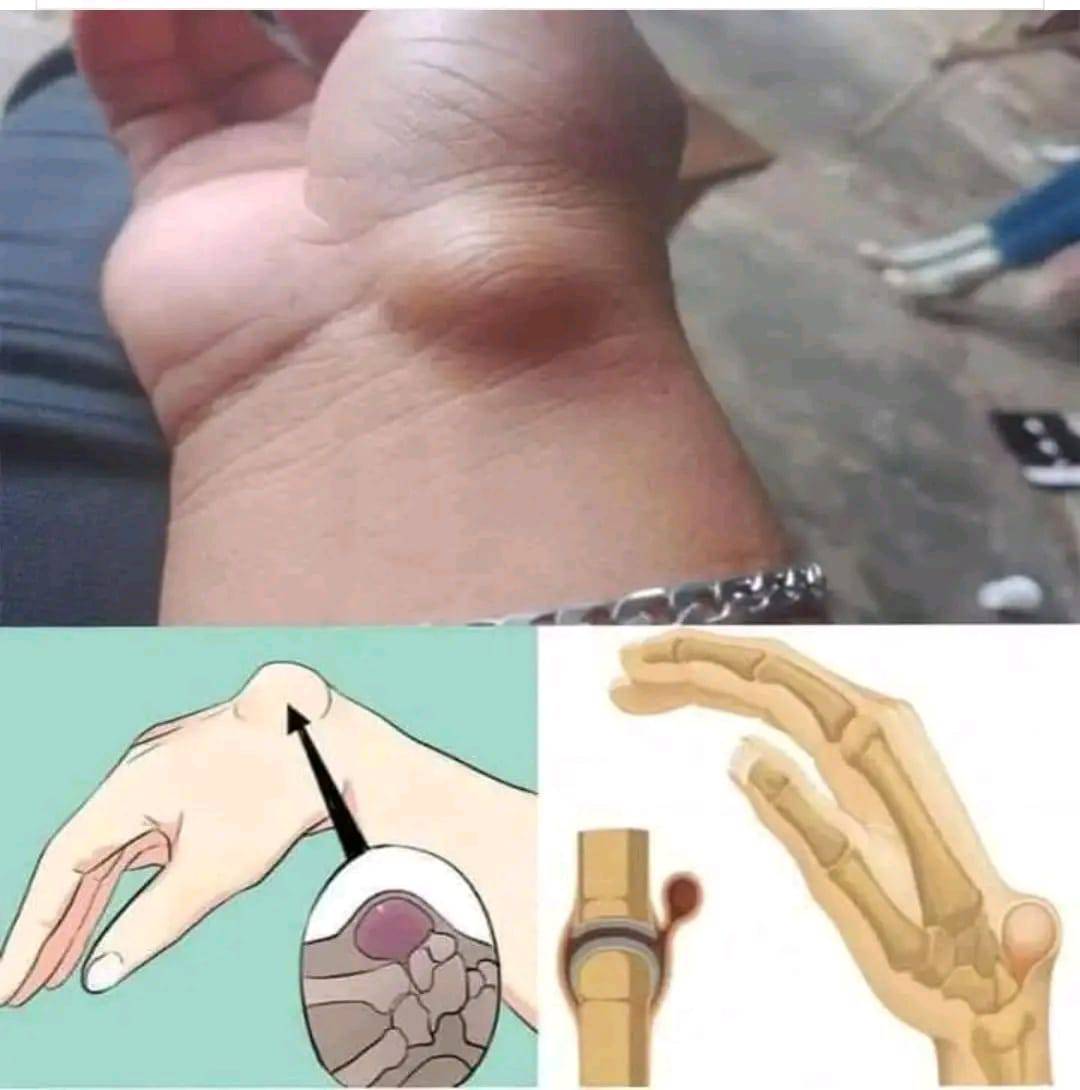
Physical Examination
The physician evaluates bruises—size, shape, color, distribution, and pattern—and looks for signs of petechiae (tiny pinpoint hemorrhages), purpura (larger non‑blanching spots), or systemic signs such as enlarged spleen or lymph nodes. Skin integrity, signs of sun damage, signs of trauma, or needle marks (in cases of intravenous drug use) are also assessed.
Laboratory Investigations
– Complete blood count (CBC) with platelet count (thrombocytopenia or anemia)
– Peripheral blood smear (platelet morphology, blasts, schistocytes)
– Coagulation panel: prothrombin time (PT), activated partial thromboplastin time (aPTT), international normalized ratio (INR)
– Liver function tests and kidney function tests
– Vitamin levels (vitamin C, K, B12, folate)
– Specific tests: von Willebrand factor antigen/activity, factor VIII/IX assays, platelet function tests
– Additional tests as indicated: autoimmune markers (ANA, anti‑dsDNA), viral hepatitis panels, HIV test, D‑dimer, fibrinogen.
Imaging and Further Diagnostics
In more complex cases, imaging may help: ultrasound of the abdomen for organomegaly, CT or MRI to locate internal bleeding, bone marrow biopsy for suspected leukemia, and skin biopsy if vasculitis is suspected.
Treatment and Management
Address Underlying Cause
Treat any identified deficiency (vitamin C or K supplementation), manage liver disease, adjust medications if needed (e.g., altering dosage of anticoagulants), and treat autoimmune or hematologic disease appropriately.
Supportive Care
Apply cold compresses early after bruising to reduce bleeding and swelling, followed by warm compresses after 48 hours to increase circulation and healing. Elevation of the affected area helps reduce swelling. Protect areas prone to injury.
Topical Treatments
Over‑the‑counter topical arnica gels, vitamin K creams, or heparinoid creams may help speed bruise resolution, though evidence varies. Gentle massage (only after the bruise has matured past the red/blue phase) may improve circulation.
Pain Management
If bruises are painful, acetaminophen (paracetamol) is preferred over NSAIDs, which may worsen bleeding. Always discuss pain relief options with your healthcare provider.
Lifestyle and Dietary Measures
Maintain a balanced diet rich in fruits, vegetables, and sources of vitamin C (e.g., citrus fruits, berries, broccoli), vitamin K (leafy greens), and protein for tissue repair. Stay hydrated. If you smoke, consider quitting, as smoking impairs blood vessel integrity. Engage in gentle strength and balance exercises to reduce fall risk, especially in elderly individuals.
Follow‑Up and Monitoring
Track bruise frequency, size, healing times, and any new symptoms. Follow up with your healthcare provider to adjust treatment, repeat lab tests, or refer to specialists (hematologists, dermatologists, rheumatologists) if needed.
Prevention Tips
See more on the next page
Advertisement